A Year in Review:
Reckoning with Loss, Rising to the Moment
By Dr. José M. Zuniga
As 2025 draws to a close, the global HIV response stands at a crossroads defined by paradox: we have never possessed more scientific knowledge, biomedical tools, or community wisdom, yet we are confronting the most destabilizing political, financial, and institutional headwinds in more than two decades. This year has made clear that progress is not linear, rights can erode, and achievements we once believed irreversible remain vulnerable. And yet, amid these challenges, the resilience and resolve of cities, communities, clinicians, advocates, and public health leaders provide the strongest evidence that our movement will not be undone.
For IAPAC, this has been a year of deep engagement with and commitment to the people and communities we serve, including our 30,000 clinician-members and the people living with and affected by HIV to whom our members deliver critical HIV services. It was also a year defined by financial hardship felt collectively across the non-profit sector, during which we were forced to embrace austerity measures and pursue creative strategies to deliver on our mission with fewer resources, including human. Even amid this strain, we took on additional unfunded mandates.
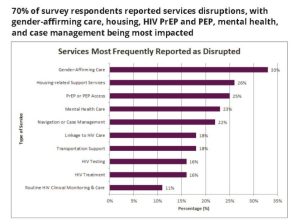
Among these mandates was the establishment of the Emergency HIV Clinical Response Task Force, which IAPAC chairs alongside our partners the American Academy of HIV Medicine (AAHIVM), Association of Nurses in AIDS Care (ANAC), GLMA, and the HIV Medicine Association (HIVMA). Together, and with support from our colleagues at Ready, Aim, Innovate, we are monitoring HIV service disruptions across the United States, documenting patterns that reveal the consequences of political retrenchment, weakened public health infrastructure, and shrinking safety nets. That we did this work without new funding is not a boast; it is a reminder that this movement has always persisted through collective will and shared responsibility.
In 2025, IAPAC also took an uncommon but necessary step into legal advocacy as one of the nine medical and public health organizations that filed Washington State Medical Association et al. v. Kennedy to challenge the politically driven removal of critical federal health data from public websites – a move that jeopardized access to evidence-based HIV information and broader public health guidance for clinicians, people living with HIV, and the American public. In September 2025, a negotiated settlement ensured the restoration of deleted webpages and data, reaffirming that science, truth, and transparency cannot be subject to ideological erasure and underscoring how access to reliable health information is foundational to quality HIV prevention, care, and treatment.
Beyond these policy and legal advocacy efforts, we also spent the year reaffirming science, solidarity, and urban leadership efforts. Throughout the year, we launched a series of virtual Fast-Track Cities townhalls, creating space for clinicians, community members, and policymakers to parse emerging data, highlight service disruptions, and surface the lived realities of HIV care in a rapidly changing political landscape. These conversations reinforced a truth we have long known: community voices remain the moral and strategic compass of the HIV response. The townhalls have also uncovered the out-of-the-box ways our communities tackle challenges – big and small – that can derail the lives of the most vulnerable among us, including transgender individuals.
We marked a moment of global solidarity with a highly successful Zero HIV Stigma Day 2025 campaign on July 21st, during which advocates, cities, clinicians, networks of people living with HIV, and partners worldwide united under the theme #HIVStigmaWarriors. The campaign inspired local dialogues, cross-sector events, and policy conversations about U=U and other key messages, reminding us that stigma continues to be both a social determinant and a barrier – and that mobilizing against it requires sustained, intersectional action. Once again, we benefited from our partnerships with Ally Wellness, GNP+, and the Prevention Access Campaign (PAC), but also solidarity with community-based organizations around the world.
In June 2026, we convened Continuum 2025 in San Juan, Puerto Rico, where almost a thousand delegates explored implementation science, health systems strengthening, quality of life, and the evolving landscape of HIV prevention and treatment. The introduction of the Primary Care and HR-QoL track reflected an overdue shift towards whole-person, whole-health approaches – an ethos now embedded within the conference framework, in addition to a new Cardiometabolic Health track to further demonstrate the importance of integrated health responses in our Continuum 2026 program.
The year also marked domestic engagement through the U.S. Fast-Track Cities 2025 Summit in New Orleans, where city and county health departments, clinicians and other service providers, community advocates and leaders, and corporate partners convened in the shadow of political attacks on public health. U.S. cities reaffirmed their commitment to scaling PrEP and ART, addressing structural inequities, and protecting LGBTQ+ communities. In addition to hosting the Summit, IAPAC presented data informed by work from the Emergency HIV Clinical Response Task Force and released an HIV policy brief with recommendations for cities, states, and clinicians to mitigate harms from upcoming Medicaid work requirements that could disrupt access to HIV and other health services.
Globally, more cities signed onto the Fast-Track Cities network, now more than 600 cities working to end their HIV epidemics and address related health challenges within the context of breaking down silos and taking a diagonal approach to addressing a broad scope of health issues with which we all contend at some point or another in our lives. We welcomed to the network Asbury Park, Köln, Mannheim, Rome, Verona, and other cities whose commitment to public health stands in stark contrast to the weakening of the multilateral framework that has historically anchored the global health response. Fast-Track Cities are practicing multilateralism in real-time.
2025 has also illuminated vulnerabilities that demand frank acknowledgment. We have witnessed a loss of critical mass at WHO, including the erosion of staff and programmatic continuity. At the same time, UNAIDS senselessly faces an existential threat, with political currents pressing towards sunsetting or radically downsizing the program by 2026. For a world where HIV continues to claim 630,000 lives a year and generate 1.3 million new infections (2024 UNAIDS estimates), such moves are shortsighted at best and dangerous at worst.
Compounding these pressures are uncertainties surrounding PEPFAR’s future, as well as the opaque “Health Cooperation Agreements” the United States is negotiating with several countries – agreements that lack clarity regarding accountability or sustainability, health data protections, and commitments to key and vulnerable populations. Meanwhile, although the Global Fund fared well in its replenishment, experience has taught us that nothing is guaranteed until the money is in the bank, particularly in a volatile geopolitical and economic climate.
But the risks extend beyond bilateral and multilateral agencies. IAPAC, along with many community and clinical non-profit organizations worldwide, is confronting the consequences of federal government retrenchment and uncertainty. Critical U.S. funding streams have been placed on hold, reduced, or eliminated. International support is increasingly unstable. And corporate funding – which has played an essential role in advancing HIV prevention, treatment, implementation science, and stigma reduction – has also diminished. While many corporate donors have doubled down on their commitment to non-profit missions, in some cases the opposite would appear to be the case due to explicit “starvation tactics” that aim to extract more output from fewer resources while signaling future disengagement.
These pressures affect the HIV services people receive, the innovations we can scale, the clinicians we can train to deliver innovations, the data we can generate to map our course, and the communities we can support without resorting to rationing. Specifically, they influence the speed at which we can respond to HIV outbreaks (they are coming!), the extent to which we can scale PrEP (no matter the hype!), the continuity of care across disrupted health systems (disruptions are real!), and the trust that communities place in institutions like ours (earned not assumed!). True to our mandate, IAPAC put out a special report in 2025 titled, Disrupt to Deliver: Reimagining PrEP, with recommendations for accelerating the pace of PrEP scale-up within the context of patient choice. But these recommendations are only text on a page if they are not actioned with robust support for all sectors responsible for advancing a cohesive, multisector HIV response.
We must also confront a persistent and uncomfortable truth: far too many people living with HIV remain undiagnosed, not on ART, or not yet virally suppressed. Treatment as prevention – now unequivocally affirmed through U=U – remains one of the most cost-effective, scalable, and immediately impactful interventions in public health, yet sustained investment in testing, rapid ART initiation, adherence support, and long-term retention in care is increasingly being overshadowed by enthusiasm for long-acting PrEP. This is not an argument against PrEP, but a call for balance. Epidemic control will not be achieved by sidelining proven fundamentals in favor of the “shiny new,” and ending HIV requires simultaneous scale-up of prevention and treatment with viral suppression for all people living with HIV at the center of our strategy.
The HIV movement has weathered adversity before, but the present moment calls for an honest accounting of the risks we face and a renewed insistence that we cannot end the HIV epidemic with weakened institutions, shrinking funding, and piecemeal support. So, since 2025 insisted on handing us both lemons and the occasional slice of cake, it is only fair that we review the challenges and opportunities it delivered – sometimes in the same breath. Following is my attempt at taking stock of both with equal parts realism and resolve.
Top 5 Challenges Moving Into 2026
- Policy reversals, attacks on LGBTQ+ rights, and budget cuts are undermining national and local HIV responses. A fragmented federal apparatus cannot sustain the scale of action required to halt rising infections and avertible deaths. As these pressures intensify, it becomes even more essential that communities – not just institutions – lead response strategies, a principle reflected in IAPAC’s integration of lived experience across 100% of our activities through our Community Advisory Board.
- The weakening of WHO’s technical capacity and ongoing threats to UNAIDS pose direct hazards to coordination, surveillance, normative guidance, and accountability. These risks are compounded by uncertainty surrounding PEPFAR’s long-term trajectory and ambiguity within the new Health Cooperation Agreements, as well as the reality that while the Global Fund’s replenishment appeared successful, nothing is certain until pledges are converted into actual resources that reach countries and communities.
- In too many countries – including the United States – PrEP uptake remains inequitable, stigma persists, and prevention infrastructure is fragile. Long-acting injectable PrEP will not scale itself; systems must be strengthened to deliver it, clinicians supported to initiate and maintain its use, and patients empowered to make informed decisions about their preferred PrEP modality.
- Reduced philanthropic and corporate commitments, austerity-driven donor landscapes, and shifts in domestic spending priorities threaten the sustainability of community-led programs and clinical services. The resulting gaps risk widening inequities and undermining epidemic control. Without support, community and clinical leadership will struggle as a stabilizing force, threatening outreach and support to vulnerable communities and disrupting HIV and other health services.
- Data blind spots and fragmented accountability are also real challenges. The ability to track incidence, monitor viral suppression, identify service disruptions, and map inequities is increasingly compromised. Without data, accountability collapses and inequities widen. In the United States, whole groups of people are being made invisible (transgender individuals) or driven underground (immigrants and undocumented individuals), masking the true impacts of bad policies and reduced resources.
Top 5 Opportunities for 2026
- Urban health leadership through Fast-Track Cities helped to ensure continuity of HIV services during the COVID-19 pandemic. Cities continue to model integration, innovation, and equity-centered approaches. Their commitment remains unwavering, and their capacity to drive measurable progress remains strong if properly resources. In 2026, the opportunity lies in scaling proven urban innovations across the broader network, allowing cities to accelerate their work through shared learning, data-driven decision-making, and coordinated multisectoral action.
- Integrating communicable diseases, NCDs, mental health, and climate-related threats allows for more resilient systems and better patient outcomes. This whole-health lens better aligns clinical pathways with the realities of people’s lives. The year ahead offers a pivotal moment to operationalize these integrated models within city health systems, transforming fragmented services into cohesive care pathways that meaningfully improve population health. This is a goal we are striving to support through our global Fast-Track Cities 2026 conference in Berlin, as well as partnerships with other urban health initiatives, including C/Can (City Cancer Challenge).
- Community-led HIV service delivery models continue to show extraordinary impact in sustaining adherence, reducing stigma, and addressing disparities. Peer networks demonstrate unique strengths in reaching those most affected by systemic inequities. In 2026, strengthening and institutionalizing these peer-led approaches across clinical and public health settings will allow for more agile service delivery. Formalizing these models within health systems – supported by sustainable financing and workforce development – will ensure they can expand reach and deepen impact over time.
- Long-acting HIV prevention and treatment options, digital health tools, and new diagnostic platforms offer transformative potential. But innovation only delivers impact when aligned with real-world experiences. The opportunity now is to build the workforce, procurement pathways, data systems, and reimbursement mechanisms required to ensure that breakthrough technologies achieve widespread and equitable uptake. Pairing innovation with implementation science and supporting the clinical, public health, and community sectors, will support us to accelerate towards real-world impact.
- Reclaiming accountability as a movement is imperative to moving forward and building back better. The HIV movement has a renewed opportunity to reclaim accountability as a collective responsibility. This moment allows us to redefine the standards against which progress is judged. By establishing clear expectations for performance across stakeholders, we can re-anchor the HIV response in measurable progress that guides investment, strategy, and trust. In doing so, we create a more predictable and evidence-driven ecosystem that protects gains, highlights disparities, and promotes accountability.
With the close of this difficult year two weeks away, the HIV response stands at a juncture shaped by institutional fragility, shrinking resources, rising political hostility, and persistent inequities. However, equally important is extraordinary innovative breakthroughs, the resilience of cities and municipalities, the strength of communities, and the determination of those who refuse to let progress slip away.
As someone who has devoted more than three decades to this work – witnessing triumphs, losses, and countless turning points – I know our path forward will be defined not by the challenges we confront but by how we confront them together. In 2026, our solidarity, our courage, and our shared accountability will determine the future we deliver for communities worldwide. Let us reckon with our loss and rise to the moment.
Dr. José M. Zuniga is President/CEO of IAPAC and the Fast-Track Cities Institute.