A Warning from the Frontlines: Protecting a Disrupted US HIV Response
By Dr. José M. Zuniga
The US HIV response stands at a perilous crossroads. After decades of progress driven by bipartisan support, scientific breakthroughs, and community resilience, the programs that could bring us within reach of ending the HIV epidemic are now under threat. In response to mounting restrictions and proposed cuts to federal funding for HIV prevention, care, and treatment, five leading professional associations joined forces to launch the Emergency HIV Clinical Response Task Force.
The Task Force – comprising the American Academy of HIV Medicine (AAHIVM), Association of Nurses in AIDS Care (ANAC), GLMA, HIV Medicine Association (HIVMA), and International Association of Providers of AIDS Care (IAPAC) – represents the clinicians, nurses, and allied health professionals who form the backbone of the US HIV response. Together, we are committed to identifying, monitoring, and addressing service disruptions that threaten the health and dignity of people living with and vulnerable to HIV.
To assess the early impact of policy and funding shifts, the Task Force conducted a national survey among its member networks. The response was sobering: 526 clinicians shared firsthand accounts of how federal policy and funding headwinds are already disrupting HIV services. The data reveal a system under strain – one where disrupted testing, prevention, and treatment services threaten the lives of the people whose members our respective Task Force organizations represent and support.
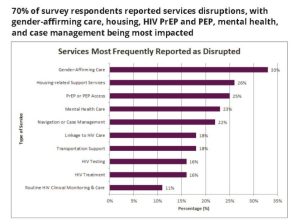
The survey findings are not abstract. They represent the lived reality of clinicians who, every day, diagnose, treat, and support people across the HIV continuum of care. As noted in the Task Force’s data brief released October 20, 2025, 70% of survey respondents reported service disruptions in their clinical settings, with gender-affirming care (33%), housing support (26%), and HIV PrEP and PEP (25%) most impacted. The populations most affected by the disruptions include transgender individuals (41%), immigrants or undocumented individuals (38%), and people experiencing homelessness or unstable housing (29%), LGBQ individuals (29%), and Latinx/Hispanic individuals (29%).
The United States has made extraordinary advances in HIV prevention and treatment, including over the last six years of the federal Ending the HIV Epidemic (EHE) initiative. Biomedical innovations like PrEP and ART for treatment as prevention or U=U have dramatically reduced HIV acquisition, transmission, and mortality. But science alone cannot sustain progress without political commitment and reliable funding. If the current trajectory continues, the goal of ending the US HIV epidemic will slip further from reach.
This Task Force’s first data offers a snapshot of what is at stake. The survey findings are both a warning and a call to action to address the urgency of now. HIV service disruptions are no longer predicted or anecdotal. Life-saving services for vulnerable communities are being disrupted, with more disruptions projected because decisions affecting people’s health are being informed by ideology – not public health rationale. For me, the message from the frontlines is clear: If we fail to act now, we face the prospect of a resurgence in new HIV infections and AIDS-related deaths.
Click here to read the Task Force’s data brief.
Dr. José M. Zuniga is President/CEO of IAPAC and the Fast-Track Cities Institute.





